
 (732) 246-1377
(732) 246-1377
 (732) 246-1377
(732) 246-1377

Heel stretch exercises can offer an effective solution for relieving foot pain and tightness. One beneficial heel stretch is the gastrocnemius heel stretch, performed by standing facing a wall with the leg to be stretched behind and toes pointing forward. Start by keeping the back heel down and the knee straight while lunging forward onto the front leg. This helps to reduce tension and friction on foot structures, ultimately alleviating foot and ankle pain. Another helpful technique is the foot pull stretch. Sit with one leg crossed over the other, and gently pull all toes back toward the shin to provide relief for plantar fascia tightness. The ball rolling exercise is accomplished by sitting with the foot resting on a golf or tennis ball and rolling it backward and forward. This has been effective in stretching the soft tissues underneath the heel and ball of the foot, which may ease pain from plantar fasciitis. Incorporating these stretches into a daily routine can significantly contribute to diminishing foot pain and enhancing overall foot health, promoting a more comfortable and pain free lifestyle. If you are experiencing foot or heel pain, it is suggested that you schedule an appointment with a podiatrist for an examination and treatment options.
Why Stretching Is Important for Your Feet
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with one of our podiatrists from Livingston Footcare. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first to determine if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising to ice and rest the foot. It is advised that you then see a podiatrist for help.
If you have any questions, please feel free to contact our office located in North Brunswick, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Debilitating foot pain is a problem for many people. But just as stretching the torso can help alleviate back pain, stretching the feet can also help mend existing foot problems and prevent future ones.
The feet, as the body’s foundation, carry the body’s entire weight and can get easily strained from overexertion. Persistent sharp pain and cramping in the feet are often common concerns. Foot pain and foot problems can be due to any number of causes, and in many cases pain may be eased without medication or doctor visits. It is always a good idea, however, to first rule out any serious medical issues with a physician.
Stretching can help relax the feet and alleviate pain, but is especially important before heavy aerobic exercise. Stretching before such activities can help you avoid experiencing painful cramps or strained foot muscles. Stretches should be performed slowly and deliberately without forceful pulling. The stretch should be held for several seconds before relaxing.
A great way to stretch out and loosen up the foot muscles while sitting is to cross one leg over the other and pull the toes carefully back without overextending. Start by resting the left ankle on the right knee. With the left hand, gently flex the left foot by pulling back on the toes. Do not pull too hard; just hard enough to feel the stretch in the arch of the foot. Then point the toes of the left foot as far as you can. Rotate the motion of pointing with pulling back on the toes. This should relax and stretch the muscles on the bottom and the top of the foot. Doing this stretch ten to twenty times should bring relief. Repeat the whole process for the other foot by resting the right ankle on the left knee.
A stretch that focuses on the often injured Achilles tendon involves standing and facing a wall with your arms out and hands flat against the wall. Step back with one foot, keeping it flat against the floor. Move the other leg forward and lean toward the wall. You should feel a stretch through the back of your leg and your Achilles tendon, but do not push yourself too much. Stop when you feel a stretching sensation, and hold for 30 seconds. Ten repetitions may be done for each foot.
Stretching the feet is important for athletes or those performing aerobic exercise, but it can also help anyone with foot pain caused by poor footwear, plantar fasciitis, or long hours standing and walking. Individuals who tend to their feet by regularly stretching every day should be able to minimize foot pain and prevent new problems from arising.
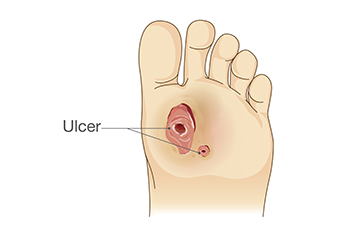
Diabetic foot ulcers pose a significant risk for individuals with diabetes, due to poor skin circulation and reduced foot sensation. Preventative measures, such as regular foot examinations and maintaining optimal diabetic control, are essential in averting these complications. Once diabetic foot ulcers develop, effective treatment becomes paramount. Typically, a protective dressing is applied, and a podiatrist plays a pivotal role in regular examination, cleaning, and redressing of the ulcer. Podiatrists may also remove hard skin hindering the healing process and prescribe padding or recommend specialized shoes to alleviate pressure. In cases of infection, oral antibiotics can be prescribed, and, if necessary, intravenous antibiotics can be administered. Surgical procedures, such as draining pus or removing dead tissue, may be required in severe infections. While many foot ulcers respond well to treatment, some may lead to severe infections or other complications. Managing diabetic foot ulcers is a long-term problem, emphasizing early intervention and meticulous care for improved outcomes and overall foot health. For help in managing diabetic foot ulcers, it is suggested that you schedule regular appointments with a podiatrist.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Livingston Footcare. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in North Brunswick, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.

Metatarsalgia, a painful inflammation in the ball of the foot, can disrupt your daily activities and hinder your mobility. This condition primarily affects the area between your toes and arch, known as the ball of the foot, where the five metatarsal bones connect to your toes. Metatarsalgia is commonly triggered by overuse injuries from participating in running and jumping activities. Other causes can include wearing ill-fitting shoes, foot abnormalities or deformities, or underlying conditions such as arthritis. The pain typically develops gradually, improving with rest, but worsening during weight-bearing activities such as standing, walking, or exercising. Symptoms may include sensations of walking with a foreign object in your shoe, a sharp burning or shooting pain, and numbness or tingling in the toes. Activities that make metatarsalgia worse can include standing for prolonged periods, running, walking barefoot, and engaging in high-impact sports. Pain in the ball of the foot arises from increased pressure on the metatarsal bones during activities like running, causing overuse and inflammation in the affected area. This abnormal stress can irritate tendons, ligaments, and cartilage around the metatarsal bones. If you are experiencing persistent pain in the ball of your foot, it is suggested that you schedule an appointment with a podiatrist for treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Livingston Footcare. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in North Brunswick, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.

Tarsal tunnel syndrome, abbreviated TTS, is a relatively rare but painful condition involving the compression of the tibial nerve as it passes through the tarsal tunnel, a narrow passageway on the inside of the ankle. The tarsal tunnel is enclosed by bone and ligaments, and when pressure is exerted on the tibial nerve within this space, it can lead to TTS. The exact causes of tarsal tunnel syndrome can vary, but common factors include injury or trauma to the ankle, such as sprains or fractures, which may lead to swelling and compression of the nerve. Overpronation, where the foot rolls excessively inward, can also place additional stress on the tibial nerve. Other factors contributing to TTS may include systemic conditions like diabetes, which can result in nerve inflammation and entrapment. Recognizing the potential causes of tarsal tunnel syndrome is essential in seeking appropriate medical care and taking preventive measures to alleviate this painful condition. If you have foot pain, it is suggested that you contact a podiatrist who can accurately diagnose and treat tarsal tunnel syndrome.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Livingston Footcare. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
The Effects of Tarsal Tunnel Syndrome
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in North Brunswick, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.

Our feet, remarkable in their complexity, house a network of 26 bones each, expertly coordinated to support our body weight and facilitate movement. These bones can be categorized into three main groups, notably the tarsal bones in the ankle, the metatarsals in the arch, and the phalanges in the toes. Tarsal bones, including the heel bone, or calcaneus, and the talus, provide stability and shock absorption. The metatarsals form the longitudinal arch of the foot and act as a lever for propulsion, while the phalanges allow dexterity and balance. Ligaments, tendons, and muscles work in harmony to control these bones and facilitate various movements. The interplay of these bones enables the foot's natural shock-absorbing mechanism, dissipating the forces generated during walking, running, or jumping. Proper alignment and functioning of these bones are essential for maintaining foot health and overall well-being. Understanding the intricate mechanics of the foot's bone structure can help us appreciate the importance of foot care and the significance of maintaining proper posture and gait. If you would like to know more about the biomechanics of the feet, it is suggested that you consult a podiatrist who can provide you with useful information.
If you have any concerns about your feet, contact one of our podiatrists from Livingston Footcare. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in North Brunswick, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.